Overtraining, Inflammation, Insufficient Repair: Scientists Shed Some More Light on the Counterproductive Triad of Ups & Downs in Testosterone, IL-6, IL-10, COX II & Co
 |
| Image 1: Part of Christian Bale's protocol to become the skinny Machinist was, you guessed it, overtraining - accompanied by undereating, the results (left) were profound. |
Update: My friend Carl Lanore from Super Human Radio happened to read this post, yesterday and as chance would have it, had a show scheduled with Brooks Kubik on the issue of Overtraining and How it Pertains to General Health, he called me and we had a nice round-table discussion on air. So, in case you are interested, here is the podcast.
Overtraining is determined by an imbalance of pro- and anti-inflammatory factorsWhile many of the results of their 11-week rodent study are not actually new (e.g. weight loss, drop in testosterone, etc. figure 1) and their significance for the average physical culturist, who won't be following an exclusively treadmill based exercise protocol are questionable, their findings pertaining to the cytokine response to overtraining could shed some light onto the underlying molecular underpinnings of both skeletal muscle atrophy and hypertrophy.
 |
| Figure 1: Study design (left) and relative changes in body weight, hemoglobin and testosterone compared to sedentary control in the overtrained rodents (data calculated based on Xiao. 2012) |
 |
| Figure 2: Changes in inflammatory and anti-inflammatory factors (left) and change in gastrocnemius weight and ratio of body weight to gastrocnemius weight in the overtrained rat immediately after the protocol (OT) or after recovery (OTR; data calculated based on Xiao. 2012) |
- IL10 is the "calming" counterpart to IL-6 and co. it acts directly on monocytes and inhibits the synthesis of pro-inflammatory cytokines such as IFN-γ, IL-2, IL-3, TNFα & Co.
- COX in particular has been identified as a necessary factor for satellite cell activity (Hill. 2003) and muscle regeneration (Bondesen. 2004)
- The inhibition of COX activity by ingestion of nonsteroidal anti-inflammatory drugs (NSAIDs) has been shown to to suppress the increase in mixed muscle protein synthesis due to exercise (Trappe. 2002)
- COX-2 null mutants also showed less macrophage invasion of injured muscle during regeneration (Bondesen. 2004), a factor about which you should have read in the Intermittent Thoughts on Building Muscle (Part II) that is a critical factor for the recruitment and "installation" of satellite cells into damaged or growing muscle tissue.
- Urokinase type plasminogen activator (uPA) promotes the migration of numerous cell types, including macrophages, activated peripheral blood monocytes, endothelial cells, smooth muscle cells, and myoblasts (Novak. 2004).
- Several studies have shown that the accumulation of macrophage the damaged muscle was impaired in uPA-null mice (Lluis. 2001; Koh. 2005), with the result being impaired repair of the muscle tissue.
- uPA increase the so-called hepatocyte growth factor, a paracrine signalling molecule that tells progenitor cells to "get going" and is required for skeletal muscle regeneration (Sisson. 2009), as well as the proliferation, migration and fusion of satellite cells (Bonavoaud. 1998; Munoz-Canoves. 1997; Fibbi. 2001) .
- the downregulation of IL-10 exasperates the inflammatory reaction to exercise induced muscle damage
- the reduction of COX II inhibits or mitigates the protein synthetic response to exercise
- low COX II and uPA levels counteract the necessary replacement of damaged, let alone the installment of new myonuclei from quiescent progenitor cells (satellite cells)
Practical implications: Questionable
Yet while the study results should have made it pretty clear and yes, this means dragging yourself to the gym with delayed-onset-muscle soreness (DOMS) that requires "treatment" with NSAIDs is no longer an option, it is of little help to determine where exactly the initially mentioned margin begins and where it ends. I believe I have given you a couple of good starting points in the Step By Step Guide to Your Own Workout Regimen, but in the end, the number of factors which will influence both the position as well as the width of this margin are so numerous that is would be unrealistic to assume that any study, rodent or human, aerobic or anaerobic, one or twelve week, ... will ever provide you with the answer to the question I know you were just about to type into the comment area of this post: "Am I already training too much? Or would it be better if..."
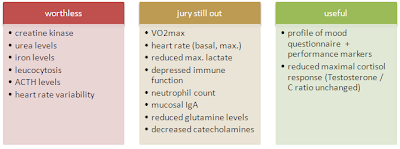 |
| Figure 3: Overview of selected biomarkers that have been investigated for their usefulness to identify over-reaching or overtraining (first published in "The Overmotivational Roots of Overtraining"; based on an overview in Purvis. 2010) |
References:
- Bonavaud S, Charriere-Bertrand C, Rey C, Leibovitch M P, Pedersen N, Frisdal E, Planus E, Blasi F, Gherardi R, Barlovatz-Meimon G. Evidence of a non-conventional role for the urokinase tripartite complex (uPAR/uPA/PAI-1) in myogenic cell fusion. J Cell Sci 1997; 110 : 1083 – 1089
- Bondesen B A, Mills S T, Kegley K M, Pavlath G K. The COX-2 pathway is essential during early stages of skeletal muscle regeneration. Am J Physiol 2004; 287 : C475 – C483
- Fibbi G, Barletta E, Dini G, Del Rosso A, Pucci M, Cerletti M, Del Rosso M. Cell invasion is affected by differential expression of the urokinase plasminogen activator/urokinase plasminogen activator receptor system in muscle satellite cells from normal and dystrophic patients. Lab Invest 2001; 81 : 27 – 39
- Hill M, Goldspink G. Expression and splicing of the insulin-like growth factor gene in rodent muscle is associated with muscle satellite (stem) cell activation following local tissue damage. J Physiol 2003; 549:409 – 418
- Koh T J, Bryer S C, Pucci A M, Sisson T H. Mice deficient in plasminogen activator inhibitor-1 have improved skeletal muscle regeneration. Am J Physiol 2005; 289 : C217 – C223
- Lluis F, Roma J, Suelves M, Parra M, Aniorte G, Gallardo E, Illa I, Rod-riguez L, Hughes S M, Carmeliet P, Roig M, Munoz-Canoves P. Urokinase-dependent plasminogen activation is required for efficient skeletal muscle regeneration in vivo. Blood 2001; 97 : 1703 – 1711
- Munoz-Canoves P, Miralles F, Baiget M, Felez J. Inhibition of urokinase-type plasminogen activator (uPA) abrogates myogenesis in vitro. Thromb Haemost 1997; 77 : 526 – 534
- Novak M L, Bryer S C, Cheng M, Nguyen M H, Conley K L, Cunningham A K, Xue B, Sisson T H, You J S, Hornberger T A, Koh T J. Macrophage-specific expression of urokinase-type plasminogen activator promotes skeletal muscle regeneration. J Immunol 2011; 187 : 1448 – 1457
- Sisson T H, Nguyen M H, Yu B, Novak M L, Simon R H, Koh T J. Urokinase-type plasminogen activator increases hepatocyte growth factor activity required for skeletal muscle regeneration. Blood 2009; 114 : 5052 – 5061
- Trappe T A, White F, Lambert C P, Cesar D, Hellerstein M, Evans W J. Effect of ibuprofen and acetaminophen on postexercise muscle protein syn-thesis. Am J Physiol 2002; 282 : E551 – E556
- Xiao W, Chen P, Dong J. Effects of Overtraining on Skeletal Muscle Growth and
Gene Expression. Int J Sports Med. 2012 May 16. [Epub ahead of print]


