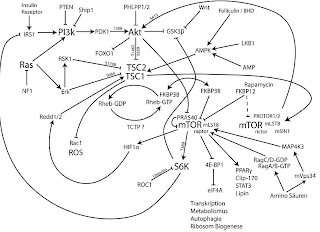
You've heard about it in several blogposts within the last week: mTOR, the short form of "mammalian target of rapamycin" and main regulator of muscle protein synthesis. Hitherto, mTOR has always been one of the good guys - getting enough protein,
leucine in particular to increase your mTOR-response is the latest advice for building muscle, which is perpetuated all over the Internet. But what if I told you that a research group from the
Quillen College of Medicine at the
East Tennessee State University in Johnson City just published a paper (
Layne. 2011) that shows that exactly this mTOR-response which is paradoxically exaggerated in patients with metabolic syndrome blunts the AMPK-mediated benefits exercise is supposed to have on insulin sensitivity.
 |
| Figure 1: mTOR signaling cascade (Wikipedia. Author: Charles Betz) |
The scientists had
10 subjects with the metabolic syndrome (MS) and 9 sedentary controls participate in an
8 week resistance exercise program with pre- and posttraining anthropometric and muscle biochemical assessments. And though the "stamina increased in both groups", the expected improvements in insulin sensitivity failed to appear in the patients with metabolic syndrome:
Insulin sensitivity increased in controls (steady-state glucose infusion rate = 7.0 ± 2.0 mg/kg · min pretraining training vs. 8.7 ± 3.1 mg/kg · min posttraining; P < 0.01) but did not improve in MS subjects (3.3 ± 1.3 pre vs. 3.1 ± 1.0 post). Muscle glucose transporter 4 increased 67% in controls and 36% in the MS subjects. Control subjects increased muscle phospho-AMPK (43%), peroxisome proliferator-activated receptor α coactivator γ (57%),and ATPsynthase (60%), more than MS subjects (8, 28, and 21%, respectively). In contrast, muscle phospho-mTOR increased most in the MS group (57 vs. 32%).
These results certainly raise the question, whether everything you read on the SuppVersity, heard on SHR and the BodyRX Show and found on various health and fitness boards was false and increased mTOR-signaling is actually something to avoid!? To cut things short: NO!
What you certainly want to avoid, though, is being sedentary and getting obese.
 |
Figure 2: Changes in body composition in kg
(data adapted from Layne. 2011) |
I also doubt that the differences in muscle fiber type, Layne et al. suggest as a possible mechanism for the absence of significant improvements in insulin resistance, cf.
Control subjects had more type 1 fibers in their vastus lateralis, whereas MS subjects had more
type 2 fibers, at a level similar to that reported in type 2 diabetes (51, 52)
are relevant in this context. What is a much more likely explanation is the combination of a
too short study period, the
absence of dietary interventions and a
relative lack of exercise "intensity", despite almost identical workloads, in the severely obese (BMI 33.7) subjects with metabolic syndrome. With a VO2Max of 23.3 ml/kg * min at baseline, their exercise capacity (emphasis on conditioning) was severely impaired if compared to the sedentary controls (31.0 ml/kg * min). Consequently their "adaptive" training program may have forced them to handle relatively high weights and thus induced comparable muscle growth (cf. figure 2), yet at the same time the concomitant reduction in in body mass and more importantly body fat (after all scientifically recognized as a self-promoting organ rather than a passive energy depot) were too small to see major changes in the obesity-induced metabolic derangement (suggested read:
Fat or Fire, What Comes First? Scientists Answer: Obesity Alone Triggers Inflammatory Signaling in Mice); supposedly, also because the obese
simply made up for the calories spent in the gym by eating more (this would also explain the greater mTOR response, if they did get at least part of their additional calories from protein sources).
If the exercise regimen had been
accompanied by an appropriate dietary intervention program and the period of study had been extended to
8 month instead of 8 weeks, I am certain one would have seen beneficial effects on insulin resistance and partial regression of all the accompanying symptoms of the metabolic syndrome. Why people (and even scientists) still cannot or do not want to understand that
single-sided (exercise or dietary instead of exercise and dietary intervention) short-term interventions cannot reverse a metabolic pathology that oftentimes took a lifetime to build up, simply eludes me.